Facial fractures from car wrecks, sports hits, or falls can leave jaws and cheeks wobbly, but maxillofacial locking plates step in like silent guardians. These clever metal strips, paired with special screws, clamp bones without squishing them tight to the hardware, letting natural healing kick in smoother and stronger. Surgeons swear by them for tricky spots where regular plates might slip or stress bones too hard, boosting recovery without extra scars or setbacks.
How Locking Plates Work Their Magic?
Regular plates hug the bone close, relying on screw pressure to grip—think of squeezing a sandwich till it squishes. Locking one’s flip that: threads on the screw heads mesh right into the plate’s holes, forming a rigid unit that hovers slightly off the bone. This “internal fixator” setup spreads chewing forces across the whole construct, dodging screw pullouts that plague thin facial bones. No need to grind plate-to-bone contact, which spares blood vessels and keeps healing cells humming.
Stability That Handles Real-Life Bites
Jaws take a beating—up to 200 pounds of bite force, grinding steak or cracking nuts. Locking plates shine here, resisting twists and bends in comminuted breaks where shards float loose. Tests show they hold 30-50% more torque than non-lockers before deforming, perfect for mandible angles or orbital rims under constant flex. In reconstructions after tumor chops, thick 2.4mm versions bridge big gaps, acting as load-bearers till grafts fuse solid.
Standout perks hit hard:
- Fixed angles stop screws from loosening under cyclic chomps.
- Less bone grinding means quicker callus buildup and fewer infections.
- One-plate wonders suffice for many fractures, slashing OR time.
Edge Over Old-School Fixation
Champy miniplates from the ’80s compressed fragments but faltered in poor bone stock—screws sank, or plates buckled. Locking systems laugh that off: no precise contouring needed, so they hug irregular surfaces from trauma swells. Studies clock 95% union rates versus 85% for non-lockers, with patients chewing soft foods days sooner. For kids or osteoporosis cases, this flexibility cuts malunions, letting faces rebuild true-to-form.
Surgical Flow and Patient Wins
Picture the op: expose the fracture via intraoral nicks or hidden eyelid cuts, plop the pre-bent plate, drill monocortically (one cortex only), and twist locking screws home—click, locked. No over-bending battles, ideal for zygoma or LeFort breaks spanning multiple planes. Post-op, folks skip weeks of jaw wiring; stability green-lights physio fast. Complication drops too—infection under 5%, hardware removal rare since nothing pokes gums.
Healing Boost from Smart Design
Biology loves this: by not strangling periosteal blood, plates spark direct osteons bridging gaps in six weeks flat. Stress shields? Minimal—the construct flexes just enough to nudge Wolff’s law, remodeling bone tougher. In free-flap jaw rebuilds, like fibula transfers, locks cradle grafts under speech strains, hitting 90% viability. Long-haul scans confirm: fused seams, no resorption, faces functioning like pre-crash.
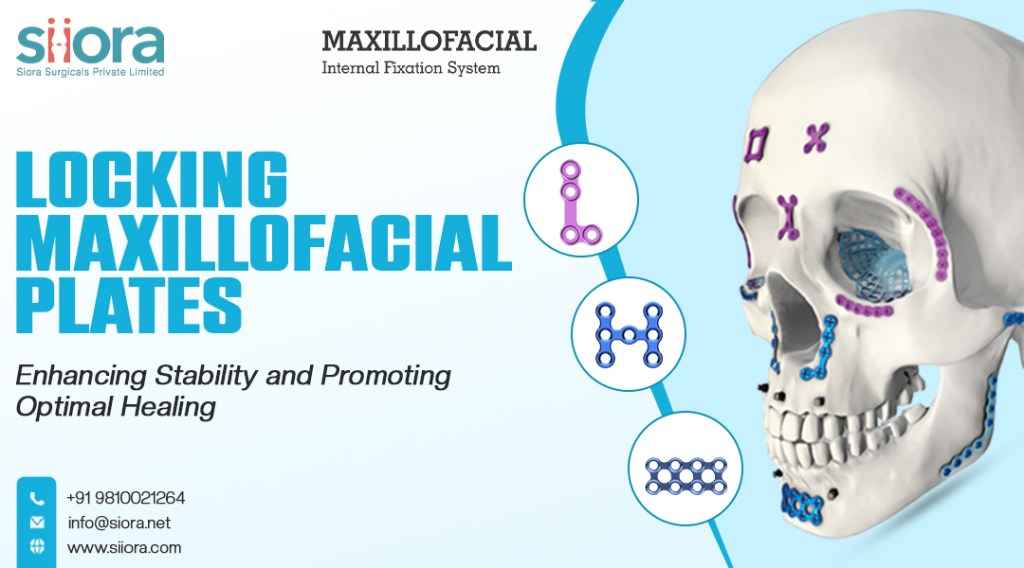
Picking Plates for Tough Cases
Not every chip needs them—simple noses take wires fine—but for atrophic mandibles, panfacial smashes, or irradiated fields, locks rule. Titanium alloys fend rust, while resorbables trial for kids. Teams mix sizes: 1.5mm for orbits, 2.4mm beasts for symphysis spans. Downsides? Pricier upfront, steeper learning for rookies. Yet payoffs—shorter hospitals, happier bites—seal the deal in busy trauma centers racing clocks.
Locking maxillofacial plates trauma implants don’t just patch; they rebuild with brains, marrying metal muscle to bone’s rhythm for scars that fade and smiles that stick.